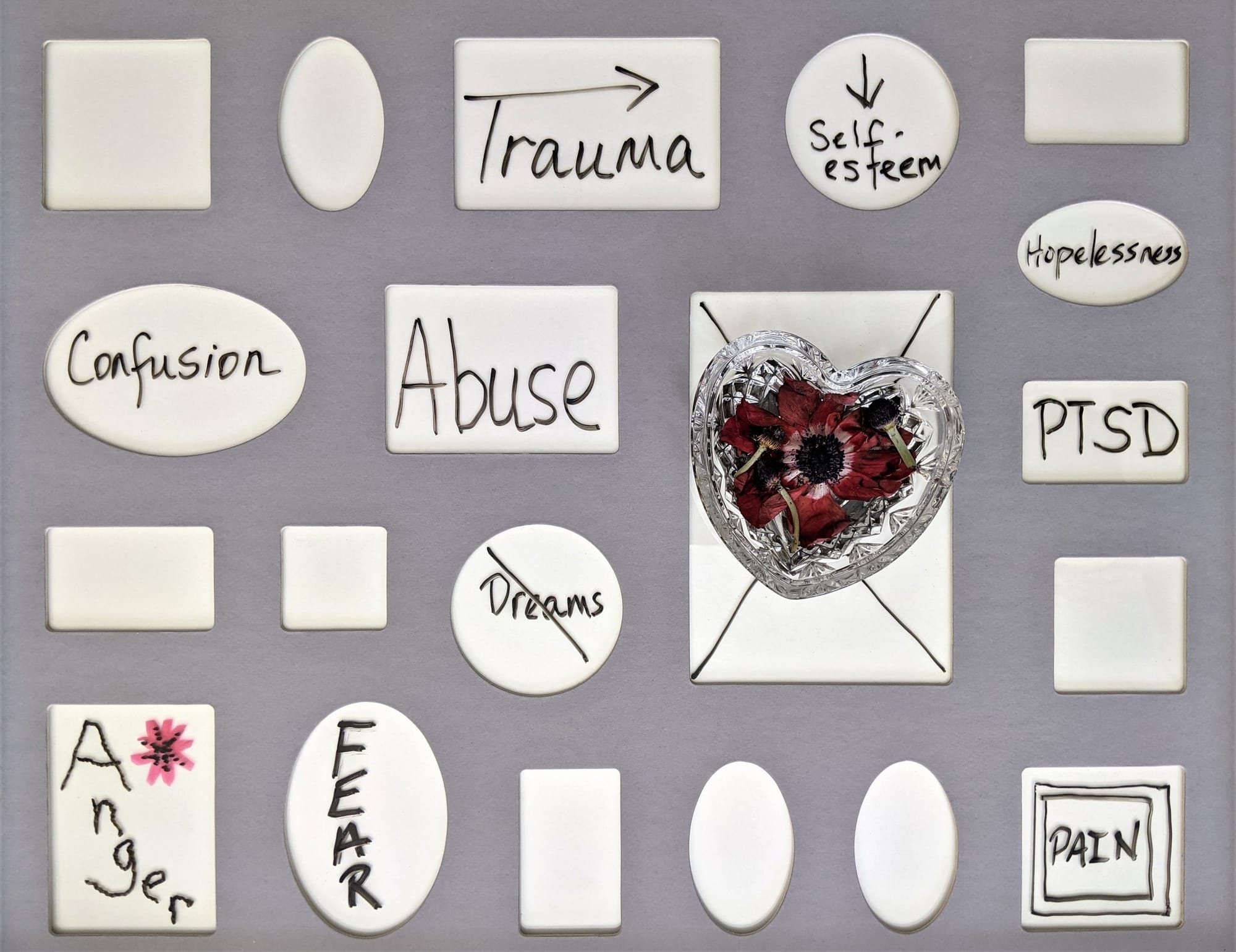
Mapping the Pathways: Trauma, Headaches, and Migraines
Introduction
The relationship between trauma, whether it be physical or emotional, and the onset of headaches and migraines has been a topic of considerable interest within the scientific and medical communities. This article aims to elucidate the pathways through which trauma influences the occurrence and severity of headaches and migraines, drawing upon the latest research findings. By understanding these mechanisms, the medical community can improve treatment options for those affected.
Methodology
To explore the connection between trauma and the development of headaches and migraines, a comprehensive review of recent literature was undertaken. The review focused on studies published in the past decade that examined the physiological and psychological mechanisms linking trauma to headaches and migraines. Both quantitative and qualitative research findings were included, with particular emphasis on studies that employed neuroimaging and psychometric testing. This multidisciplinary approach ensured a holistic view of the subject matter.
Results
The reviewed studies highlight several key findings:
- Neurological Changes: Trauma, especially when chronic, can lead to alterations in brain structures associated with pain regulation, such as the thalamus and cortex. This can sensitize individuals to pain, increasing the frequency and intensity of headaches and migraines.
- Psychological Impact: Psychological trauma can exacerbate the perception of pain and can be a significant factor in the transformation of episodic migraine into chronic migraine. Stress associated with trauma can also trigger the release of certain hormones that affect pain sensitivity and inflammation.
- Genetic Factors: There is evidence to suggest that genetics may play a role in an individual's vulnerability to developing chronic headaches or migraines following trauma. Specific gene variants related to pain and stress regulation have been associated with increased sensitivity to headaches post-trauma.
- Hormonal Fluctuations: Research indicates a link between hormonal imbalances triggered by both physical and emotional trauma and the onset of migraines, particularly in women. Changes in estrogen levels, for example, have been shown to affect migraine frequency and intensity.
Discussion
The findings from the reviewed studies paint a complex picture of the interplay between trauma and headaches/migraines. It is clear that both physical and psychological traumas can lead to significant changes in brain structure and function, affecting pain perception and regulation. Moreover, the impact of trauma is not only immediate but can also lead to a long-term predisposition to experiencing headaches and migraines, highlighting the importance of early intervention.
The role of stress hormones and genetic factors in mediating the relationship between trauma and headaches/migraines suggests potential targets for therapeutic intervention. Treatments that aim to mitigate stress responses or address hormonal imbalances may prove effective in reducing the frequency and severity of headaches in individuals experiencing trauma.
Futures research should aim to delineate more clearly the pathways connecting trauma with headaches and migraines. Specifically, longitudinal studies tracking individuals pre- and post-trauma could provide invaluable insights into the temporal dynamics of the development of headaches and migraines. Furthermore, the exploration of genetic predispositions and their interaction with environmental factors could elucidate individual susceptibility to trauma-induced headaches.
In conclusion, the research reviewed suggests a significant link between trauma and the development of headaches and migraines, mediated by a variety of physiological, psychological, and genetic factors. While treatments currently focus on managing symptoms, greater understanding of these underlying mechanisms could pave the way for more effective and targeted therapies. Ultimately, recognizing the role of trauma in headaches and migraines underscores the importance of a holistic approach to treatment, incorporating both medical and psychological support to address the multifaceted nature of these conditions.